Chapter 6 Metabolic alkalosis (& chloride homeostasis)
6.1 Causes of a metabolic alkalosis
The causes of a metabolic alkalosis can be classified as being either due to chloride depletion (and therefore chloride responsive) or due to other causes (chloride resistant) (Luke & Galla, 2012).
| LOW ECF VOLUME = CHLORIDE-DEPLETION / CHLORIDE-RESPONSIVE | GI chloride loss | vomiting / NG losses |
| GI chloride loss | colonic villous adenoma / congenital chloride diarrhoea / high-volume ileostomy (rare) | |
| loop / thiazide diuretics * | ||
| Bartter / Gitelman * | ||
| NORMAL ECF VOLUME = CHLORIDE-RESISTANT | renal H + loss | true mineralocorticoid XS (low-renin / high-renin) |
| apparent mineralocorticoid XS (and Liddle’s) | ||
| Cushings | ||
| post-hypercapnic alkalosis (UCl < 10 mM) | ||
| milk-alkali syndrome | ||
| hypokalaemia |
* in chloride-responsive states UCl < 10 mM except where chloride is being lost in the urine (i.e. diuretics / Gitelman / Barrter syndrome).
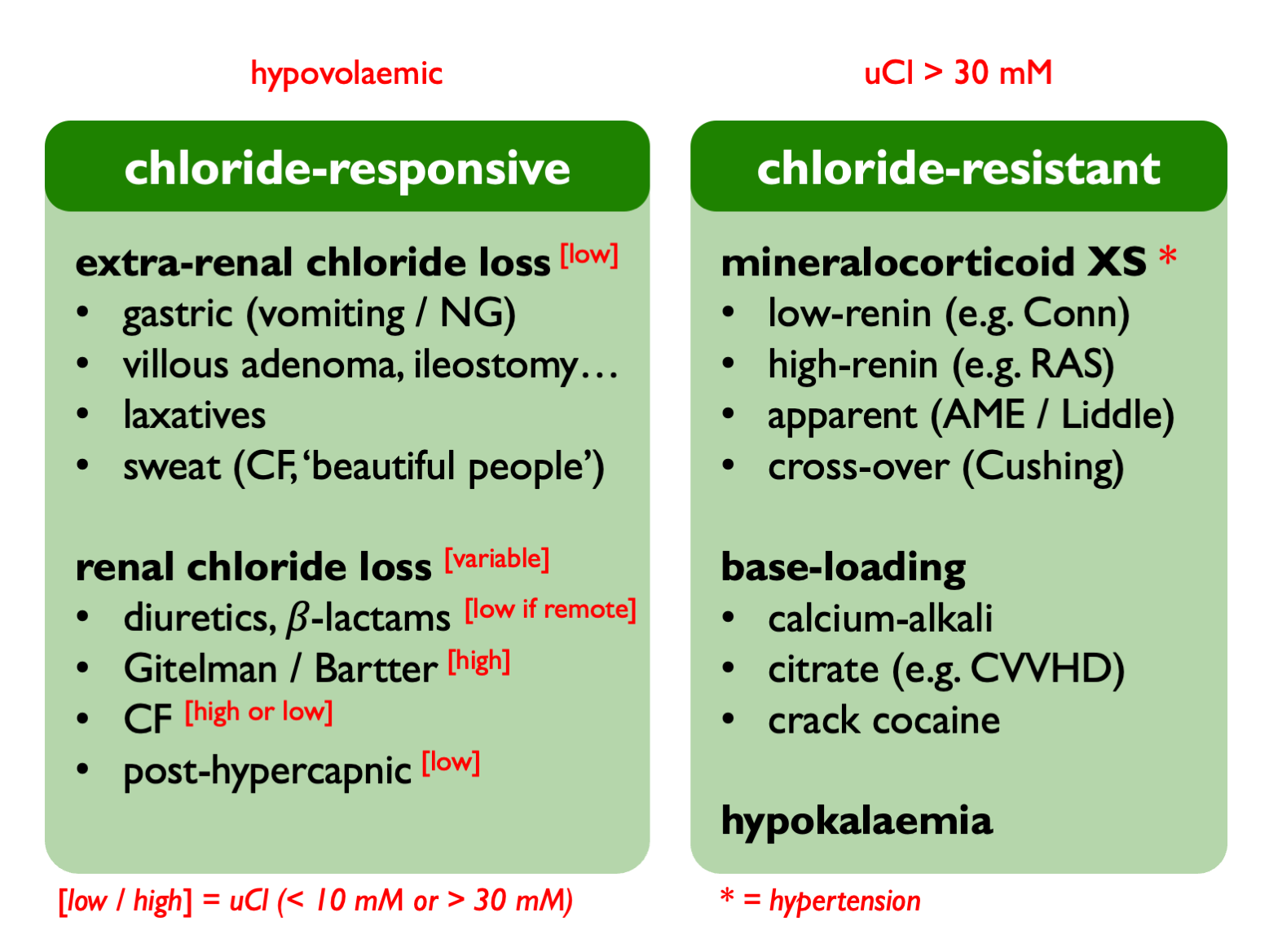
Perhaps a more useful classification would be:
- Pendrin-dependent with volume depletion = extra-renal chloride loss
- ENaC-dependent with volume depletion = renal chloride loss (secondary aldosteronism)
- ENaC-dependent with volume expansion = primary mineralocorticoid XS
- base-loading
Initial diagnostic work-up includes checking volume status, blood pressure, serum chloride and urinary chloride. Checking renin and aldosterone levels then helpful if suspected mineralocorticoid XS.
As a general rule, extreme alkalosis (HCO3 > 45 mM) can only be due to vomiting (and consider pyloric stenosis / Zollinger Ellison syndrome).
6.1.1 Specific syndromes and their mechanisms
Cystic fibrosis: loss of chloride in sweat and / or downregulation of renal pendrin (so uCl may be high or low).
Post-hypercapnic alkalosis: occuds when chronic hypercapnoea is abruptly corrected - usuall in the context of mechanical ventilation. Chronic increase in renal HCO3 reabsorption and ammoniagenesis leads to loss of urinary NH4Cl. Therefore induces a low-Cl state that requires Cl resuscitation to correct.
Pendred syndrome (AR): no acid-base disturbace at baseline but susceptible to alkalosis when provoked (e.g. by thiazides).
Calcium-alkali syndrome (formerly ‘milk-alkali’): triad of hypercalcaemia, alkalosis, AKI. Caused by ingestion of large quantities of calcium (+/- alkali); often exacerbated by thiazides. Inhibition of CaSR in TALH causes salt-wasting (and hence chloride depletion and secondary hyperaldosteronism) and alkalosis stimulates Ca2+ reabsorption through TRPV5 in DCT. So a vicious cycle; abort with IV NaCl.
Crack cocaine: sometimes made with drain cleaner.
Hypokalaemia: associated with alkalosis because of a common underlying cause (e.g. hyperaldosteronsim), cell shifts and / or hypokalaemia stimulating ammoniagenesis.
6.2 Chloride
UCl NR = 100 – 250 mmol / 24 hrs
In chloride-responsive alkalosis, UCl < 10 mM:
- vomiting
- villous adenoma
- congenital chloride diarrhoea
- recent diuretics (pause on clinic day in surruptitious use)
In chloride-resistant alkalosis UCl > 10 – 30 mM (and also if chloride loss is due to diuretics / tubulopathies).
UCl is persistently low after vomiting and is therefore a useful test for surreptitious vomiting.
6.2.1 Chloride-depletion alkalosis
In chloride depletion, reduced ECF volume leads to reduced GFR (less filtered NaHCO3) and increased Na reabsorption. Thus NaHCO3 reabsorption is increased. Increased distal Na reabsorption leads to increased acid excretion. Therefore, after vomiting, an acid urine is produced (paradoxically) in the face of a metabolic alkalosis. Treatment is volume expansion with NaCl and correction of hypoK.