Chapter 12 Hypokalaemia
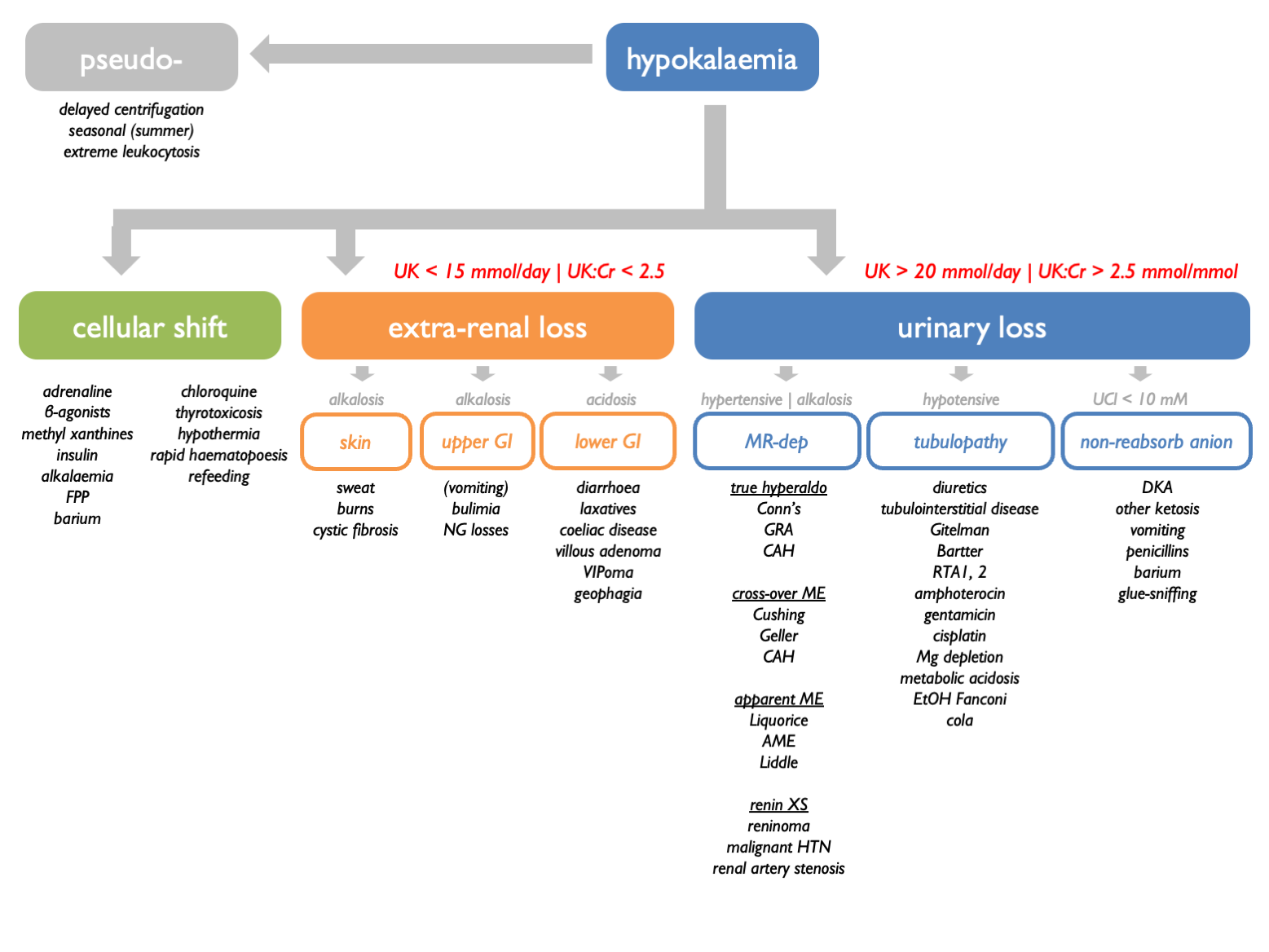
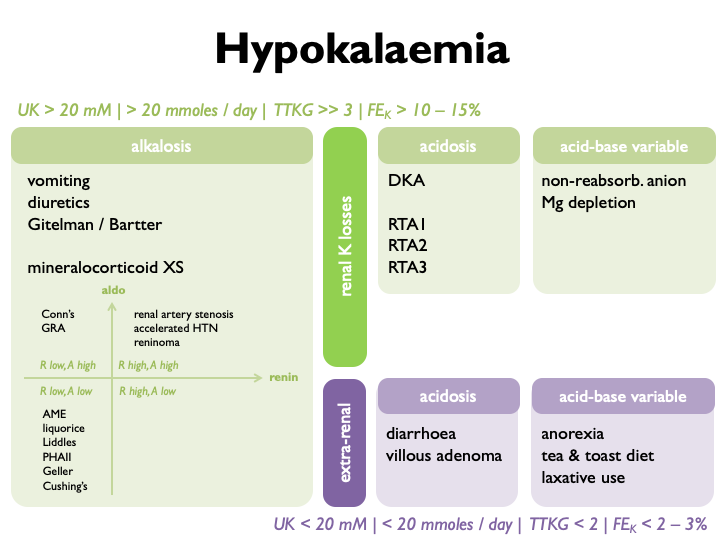
12.2 Causes of K loss
| RENAL | with metabolic alkalosis | vomiting |
| with metabolic alkalosis | diuretics | |
| Gitelman | ||
| Bartter | ||
| true mineralocorticoid XS | ||
| apparent mineralocorticoid XS | ||
| RTAI | ||
| RTAII | ||
| RTAIII | ||
| DKA | ||
| Mg-depletion | ||
| non-reabsorbable anion | ||
| EXTRA-RENAL | with normal acid-base | anorexia |
| tea & toast diet | ||
| laxative abuse | ||
| diarrheoa | ||
| villous adenoma |
12.4 Vomiting
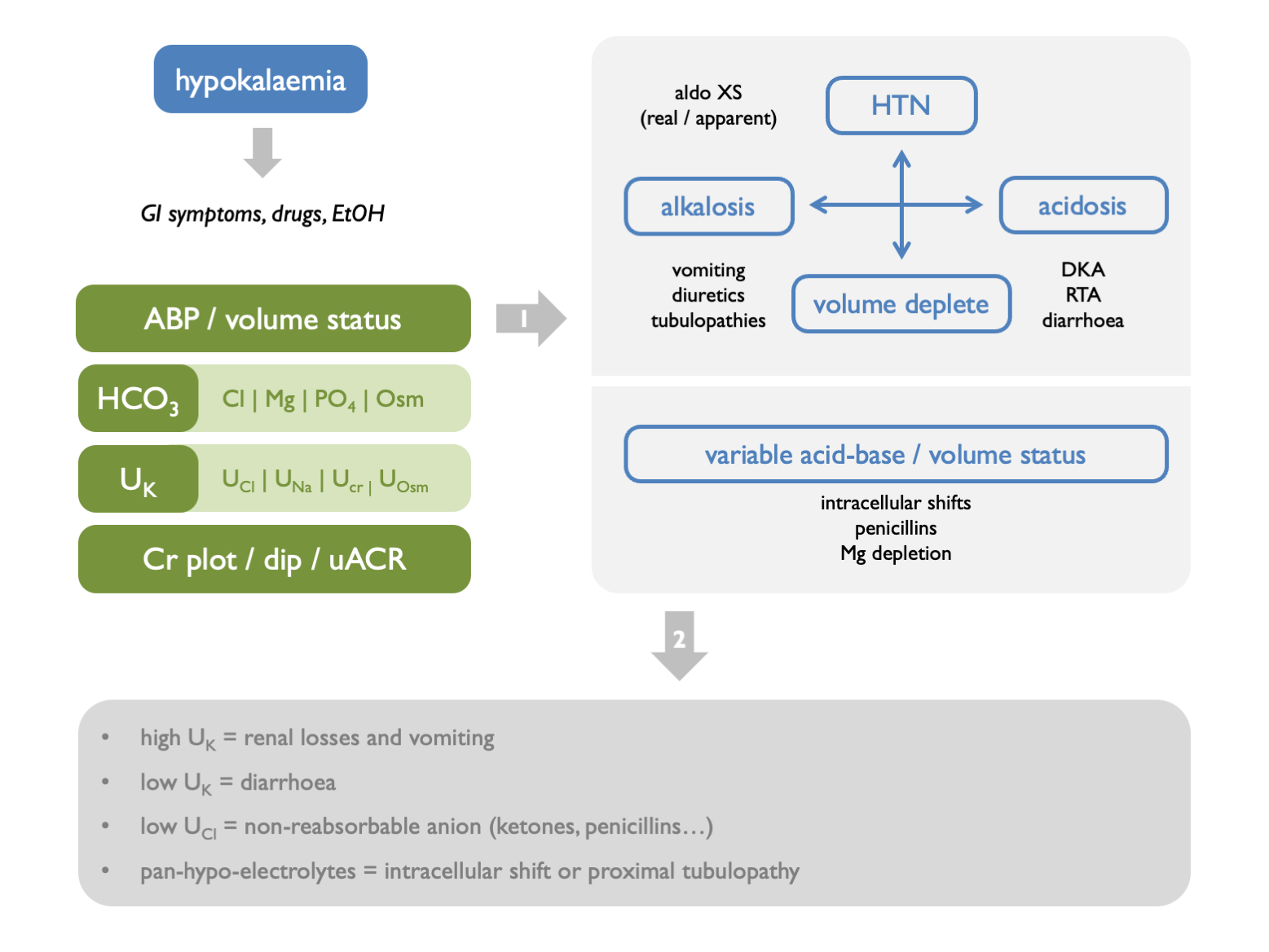
In vomiting, K is lost through extra-renal and renal routes. Volume contraction stimulates aldosterone; contribution for chloride depletion and bicarbonaturia. A urinary pH and UCl may be informative.
The classical differential diagnosis for unexplained hypokalaemia when surruptious vomiting / laxitive use is suspected is as follows:
| serum pH | UNa | UK | UCa | |
|---|---|---|---|---|
| laxative use | acidosis | < 10 mM | < 20 mM | |
| vomiting | alkalosis | < 10 mM | < 20 mM | < 25 mM |
| diuretic use | alkalosis | > 10 mM | > 20 mM | < 25 mM |
| Bartter | alkalosis | > 10 mM | > 20 mM | > 40 mM |
Eating disorder suggested by alternating alkalosis (vomiting) and acidosis (RTA from hypokalaemic nephropathy).
12.5 Non-reasbsorbable anions
Hypokalaemia can be due to renal tubular K secretion in the presence of a non-reabsorbable anion (classically IV penicillins). Look for low U.Cl and treat with IV 0.9 % NaCl. Exacerbated in volume depletion (stimulates aldosterone).
12.6 Hypokalaemic periodic paralysis
AD inheritance. Thought to be caused by K shifts between ICF and ECF. Associated with thyrotoxicosis in oriental males aged 20 – 50 yrs (in which case high risk of arrhythmias). In this case, treating the thyrotoxicosis will prevent paralysis (as will propranolol).
Triggers:
- sleep
- glucose / insulin / large CHO meal
- EtOH
- anxiety
Treatment:
- attacks IV K supplements
- prophylaxis K supplements & K-sparing diuretics